Hospitals and other healthcare providers collect data on just about every aspect of a patient’s stay, including how long they had to wait, how long they stayed, what medications and treatments they received, whether beds were available in the appropriate ward, and whether they were ultimately satisfied with their care. Healthcare dashboards collect all of this information. They also integrate a wide range of financial, supply chain, and staff data to provide a holistic view of the healthcare system. This information not only can enhance provider decision-making and improve patient care, but it also helps hospitals and healthcare institutions manage their financial health.
What Are Healthcare Dashboards?
Much like the dashboard in a car, a healthcare dashboard is an information resource that collects, analyzes, and displays real-time data in a user-friendly graphic format. And just as the car’s dashboard is designed to help drivers drive safely, healthcare dashboards guide its users—including healthcare administrators and executives, clinicians, supporting staff, and even IT professionals—to make solid decisions that lead to the best possible patient and business results.
Healthcare provider dashboards draw their information from a variety of sources, including financial, procurement, and supply chain applications, check-in systems, electronic health records, patient-monitoring systems, wearables, laboratory information systems, pharmacy management systems, insurance claims databases, and direct patient inputs. They can be tailored to specific healthcare settings, such as outpatient surgery centers or transitional care facilities. They can also be customized for specific subsets of patients, such as those receiving perinatal care, or to track the impact of an unfolding healthcare crisis, such as the COVID-19 pandemic. This flexibility allows healthcare providers to zero in on the metrics that matter most to their areas of focus.
Key Takeaways
- Healthcare dashboards gather, process, and logically display information from multiple sources, enabling informed decision-making.
- Healthcare dashboards assist organizations in tracking and managing insurance claims and eligibility, patient billing, and inventory.
- By monitoring essential performance metrics, they also highlight opportunities to cut costs and increase revenue.
- Crossroads Health, and AyurVAID Hospitals are among many healthcare organizations that have benefitted by using dashboards.
Why Are Dashboards Important in Healthcare?
Hospitals, clinics, hospices, and other healthcare providers are under enormous financial pressure as labor and other healthcare costs continue to soar and alternative sources of care emerge (think urgent care centers and pharmacy providers). It’s critical that they collect and analyze data on every aspect of their businesses to improve their services and internal operations, lower costs, and ultimately boost their bottom lines.
As a result, healthcare dashboards have become invaluable sources of business intelligence, aggregating real-time data from multiple sources and presenting it in easily interpreted formats. Business leaders are then equipped with the information they need to make informed decisions that improve operations, quality of service, and overall financial performance.
For example, without a dashboard an administrator would need to access three separate systems for data about emergency room wait times, ward occupancy rates, and staffing levels. Not only is that time-intensive, but it makes it difficult to spot correlations—such as a relationship between excessive ER wait times and crowded wards—let alone take corrective actions. Dashboards consolidate all of that information in one place, expediting the decision-making process. The administrator might decide to reassign nurses from elsewhere in the hospital to the ER, identify patients in other departments who are nearing discharge status, and instruct department heads to expedite their release to free up beds to accommodate new admissions.
Who Benefits from Using Healthcare Dashboards?
Healthcare dashboards offer value to a wide circle of users, both within and outside of the healthcare setting. Among them:
- Healthcare executives and administrators use dashboards to monitor admission rates, treatment outcomes, staffing levels, expenditures, and other data that can help them forecast trends, identify areas of overspending, compare the facility’s performance to that of competitors, and more.
- Billing departments and insurance companies rely on dashboards to monitor charges, payments, and claims processing and rejections.
- Patients and their families turn to dashboards or online portals to help them choose doctors, follow the progress of treatment plans, monitor prescriptions, view test results, track charges, and more.
- Government agencies and public health officials use dashboards to help them monitor the quality, safety, and financial standing of hospitals and other healthcare organizations, as well as to analyze public health data to improve their policymaking and responses to health crises.
- Front-line healthcare providers use dashboard data to make diagnostic and treatment decisions.
These broad applications can be supplemented by tools that mine subsets of data more deeply. For example, if a healthcare dashboard flags an uptick in the number of patients not showing up for their appointments, the organization might integrate an automated patient reminder system to reduce its no-show rates.
4 Key Features of Healthcare Dashboards
An important attribute of healthcare dashboards is that they can be customized as needed. But some capabilities are so integral to running a healthcare organization that they form the backbone of dashboards across healthcare settings and sites.
-
Claims Management
Few businesses face the complex financial realities of healthcare providers, which not only determine a patient’s course of treatment, but also (in conjunction with insurance companies and government guidelines) the charges for that treatment, as well as how to code that treatment when submitting a claim. In addition, they often serve as the intermediary between patients and their insurers. And, of course, providers want to ensure that they receive what they’re due.
A healthcare dashboard is ideally suited to simplifying claims management through the real-time tracking of key performance indicators (KPIs). They provide healthcare providers with the ability to monitor charges and payments, by date and insurer; observe trends in claim denials; and manage days in accounts receivable (also known as days sales outstanding). By highlighting metrics, such as average days to bill and collectability percentage, healthcare dashboards can help organizations assess their financial processes. Tracking claims by such factors as location, physician, and insurer further helps hospitals pinpoint areas in need of improvement, thus minimizing the need for time-consuming appeals and fostering a more efficient billing process.
-
Patient Billing
For healthcare providers, the receipt of payments from patients can significantly lag behind the payments made by insurers. Because healthcare can be very expensive—particularly for emergency room care and hospital stays—many patients opt to pay what they owe over time. Indeed, the Commonwealth Fund 2023 Health Care Affordability Survey found that 32% of Americans carry medical or dental care debt. In fact, hospitals may not receive final payments until months or even years after services are provided.
That leaves billing departments responsible for tracking a lot of outstanding balances—a process that is both time-consuming and tedious without the help of a healthcare dashboard. Dashboards can track critical KPIs—such as total and current accounts receivables—which are displayed in visual format for an at-a-glance understanding. Dashboards also make it possible for billing departments to automate formerly manual tasks, such as determining which accounts to send to collection, to streamline the process and help improve cash flow.
Automation can also improve billing accuracy because it eliminates the potential for human error every time a new charge, adjustment, or payment is entered into the system. For patients, dashboards provide visibility into their billing information and help them manage their expenses.
-
Insurance Eligibility Verification
Through integration with insurance company or third-party clearinghouse systems, healthcare dashboards can quickly verify a patient’s insurance coverage and the details of that coverage. This accelerated process benefits providers, patients, and insurers alike.
- Providers: A healthcare organization can instantly check if a patient’s insurance plan covers a particular procedure. This proactive approach not only protects the organization from revenue loss from denied claims, but it also improves the company’s financial health by ensuring a steady cash flow.
- Patients: Patients can be informed during the registration process about their coverage limits—copays, deductibles, etc.—for a scheduled consultation or procedure. This helps them to understand and plan for any potential out-of-pocket costs. It can also spare patients from “surprise” bills that can result in complaints or, worse, prompt patients to change providers.
- Insurers: Insurance companies benefit from the reduction in improper claims submissions, as the dashboard verification process helps ensure that only eligible services are claimed, leading to more efficient claims processing and lower administrative costs.
-
Inventory Management
Healthcare facilities manage a vast array of inventory, including medications, surgical supplies, medical devices, personal protective equipment, patient gowns, bedding, and much more. Effective inventory management is crucial. Errors can lead to critical shortages or wasteful overstocking.
Healthcare dashboards help improve inventory management by providing real-time visibility into supply levels and automating alerts for restocking. They track usage rates and highlight expiring items. Additionally, dashboards facilitate regulatory compliance by monitoring controlled substances, and they offer customizable views for various inventory categories, enhancing operational decision-making.
Relying on a dashboard can also directly and indirectly improve the bottom line by cutting down on paperwork, improving accuracy. and boosting efficiency.
Benefits of Implementing Healthcare Dashboards
Healthcare professionals face relentless pressure to lower costs, raise operational efficiency, and improve patient services. Dashboards are designed to help.
-
Streamline and structure data: Healthcare dashboards centralize data from multiple sources, eliminating the challenge of managing scattered and potentially redundant information stored in multiple formats. For example, a dashboard set up for a hospital inventory manager would likely reflect stock levels; usage rates across multiple departments; supplier performance, such as delivery times and order accuracy; and financial data, such as item costs and total expenditures. A dashboard not only consolidates that data, but it could also be designed to automatically send alerts when critical supplies run low or a supplier fails to meet a delivery deadline.
-
Optimize operational efficiency: Operational efficiency directly impacts patient care, resource allocation, and financial performance. Consider an operating room. It’s key revenue-generating department for a hospital, so the ability to see as many patients as possible is key. Dashboards that feature such real-time metrics as utilization rates, scheduled surgeries, turnover times between surgeries, surgeon and staff availability, and actual versus estimated times required for each surgery help administrators achieve that goal. For example, by using the dashboard to track the costs of each procedure (including staffing, materials, and equipment), administrators can see which procedures are more costly than expected, investigate the reasons, and then determine corrective measures.
-
Increase revenue potential: By mining and organizing data, dashboards can help organizations identify opportunities to cut costs and generate more revenue.
One obvious way for a healthcare company to bring in more revenue is to see more patients. Dashboards can offer insights into patient demographics, what prompted them to seek care, when patients are seen, and the length of a typical appointment. Suppose a doctor who practices telemedicine has been scheduling patients for 30-minute appointments, but her dashboard shows that the average appointment lasts about 15 minutes. With that insight, the doctor could trim the amount of time allotted for each appointment and therefore triple the number of patients being seen.
Similarly, a dashboard for a dental practice might show that patients aren’t coming for their second annual cleanings, even though their insurance allows for it. The practice could create an email campaign to promote the value of that second cleaning and increase the scheduling of those lucrative visits.
-
Identify opportunities for growth: Realizing the full potential of existing services and facilities will yield additional revenue. But after that, growth must come from new services or facilities. Dashboards can help identify these opportunities. For example, some dashboards incorporate market data and information about competitors. By comparing their own performance against market trends, healthcare organizations can identify a need to capture more market share or introduce new services to stay competitive. Some dashboards monitor referral sources and partnerships. If a healthcare system sees that referrals from certain primary care practices lead to high volumes of patients, it may consider formal partnerships or broader collaborations. Dashboards also can track the usage of new technologies, treatments or methodologies. If the data shows that any of these innovations are boosting outcomes or reducing costs, organizations can increase investments in those areas.
-
Predict trends: By mining and sorting data, dashboards can help administrators analyze trends. For example, analyzing historical information by date may reveal an uptick in visits at a chain of walk-in clinics during winter months, when patients seek treatment for respiratory infections. As a result, the chain would likely increase staffing during those months and then reduce it during warmer months, when caseloads decrease.
More broadly, dashboard data could reveal that a hospital’s population is steadily aging. In response, the hospital could proactively invest in geriatric services to prepare for anticipated demand. Dashboard information dramatically strengthens forecasting.
-
Enhance patient care: Poor bedside manners, long wait times, terrible food, and dirty facilities can damage a healthcare organization’s reputation and drive patients away. Dashboard data can help. For example, administrators can use top-level data to track staffing-to-patient ratios and make adjustments so that patients receive the proper attention. Additionally, dashboards provide real-time tracking of medical supplies, ensuring that patient care is never disrupted by shortages. They also track staff performance and patient satisfaction, identifying areas where targeted training could enhance service delivery and the patient experience. For example, a dashboard showing consistently long patient wait times in a certain department could lead to process improvements that enhance patient throughput.
-
Facilitate informed decision-making: By integrating data from various sources and simplifying data interpretation, healthcare dashboards give decision-makers at all levels the insights they need to make timely, informed decisions. For example, if a dashboard shows that certain diagnostic tools are underutilized, a hospital could decide to reallocate them to another department.
10 KPIs to Include in a Healthcare Dashboard
The value of a healthcare dashboard is only as good as the data it yields correlates to the business’s specific goals. For that reason, healthcare organizations should determine their KPIs before building a dashboard, giving due consideration to the requirements of different facilities, departments, and specialties.
-
Patient Satisfaction Score
Unhappy patients are likely to change providers and discourage potential patients through negative online reviews or word of mouth. Although treatment outcomes are typically the primary determinant of patient satisfaction, other elements, like wait times, staff competence, and facility amenities, also shape patient perceptions. Surveys are the main tool for gauging satisfaction. A patient satisfaction score (sometimes called a patient perception score) represents the average of the survey responses, offering a quantifiable measure of patient experience.
-
Average Patient Wait Time
Patients can spend a lot of time waiting, whether it’s to see the doctor during an office visit, for triage in the emergency room, between tests in the ER, and so on. Average patient wait time is typically calculated by dividing the total time patients have waited by the number of patients. This KPI can be tracked and analyzed through healthcare dashboards to help identify trends and improve service efficiency.
-
Length of Stay (LOS)
This KPI tracks how long an admitted patient stays in the hospital, averaged across all patients during a specific time period. Based on extensive historical LOS data, insurers often base reimbursements on the expected LOS for different diagnoses — which means hospital stays that exceed expectations can reduce an organization’s bottom line. They can also lead to complications, such as patients acquiring infections in the hospital, that keep them there even longer.
By monitoring LOS, hospitals can benchmark their status against national averages, identify inefficiencies, and implement process improvements to optimize patient flow and enhance care outcomes.
-
Gross Revenue
Gross revenue is an organization’s total amount of revenue before any deductions, expenses, or adjustments are made. Although tracking gross revenue by itself isn’t enough for effective financial management—for example, it doesn’t reveal anything about cash flow or profitability—it still offers value in making key decisions. For example, an increase in a hospital’s gross revenue may indicate growing demand for its services, which can drive expansion plans. By knowing the revenue generated from different services, healthcare organizations can allocate resources more effectively to high-performing departments or identify areas that may require additional investment. Gross revenue can also inform pricing strategies, budgeting, and forecasting, as well as rate negotiations with insurers.
-
Net Revenue
Net revenue is the income that remains from gross income after accounting for deductions, such as discounts, returns, and allowances. This KPI demonstrates an organization’s true sales performance. Tracked over time, changes can indicate growth or decline in the company’s core business. In practice, if a dashboard shows that a hospital’s gross revenue from surgical procedures is high but net revenue is lower than expected, it may point to underlying issues, such as too many discounts or insurance underpayments. A decline in net revenue might also indicate billing inefficiencies or payment delays, prompting review and refinement of billing practices. Additionally, consistently low net revenue from certain payers—insurance companies, Medicare/Medicaid, etc.—could lead to renegotiations of contracts to ensure fair compensation for services rendered. For nonprofit hospitals, net revenue is key for maintaining tax-exempt status and demonstrating that profits are being reinvested into patient care and community services.
-
Cost Per Treatment
A typical hospital patient likely receives more than one treatment during his or her stay. The cost-per-treatment metric identifies and totals the direct and indirect costs of each, divided by the number of treatments. Direct costs include staff time and the medical supplies, medications, and equipment used. Indirect costs include facility maintenance and administrative overhead. Cost per treatment is useful for analyzing the efficiency and cost-effectiveness of individual procedures.
-
Claim Denial Percentage
Also known as the claim denial rate, claim denial percentage quantifies the submitted claims that insurance companies deny to pay a healthcare organization in a specific time period. Denial can occur for several reasons, including data-entry mistakes, lack of preauthorization, billing or coding errors, or failure to meet payer-specific documentation requirements. Claim denials can disrupt a hospital’s cash flow, and they can incur additional costs related to time spent correcting errors; missed opportunities; and financing fees if borrowing money became necessary. Healthcare dashboards can go a long way toward helping billing departments spot denial patterns and take corrective action.
-
Reimbursement Rate
One of the challenges of healthcare finance is that the amount an organization is paid by insurers is rarely the same as what is billed. The reimbursement rate captures the amount the provider actually collects after the billed amount is adjusted through negotiations, contractual agreements, and deductions. While the claim denial rate impacts cash flow, the reimbursement rate impacts revenue. As previously mentioned, a discrepancy between high gross revenue from procedures and lower-than-expected net revenue may signal inadequate insurance reimbursements.
-
Operating Profit Margin
Operating profit margin measures the percentage of revenue left after a business deducts its operating expenses and cost of goods sold. In essence, this KPI measures how well a healthcare organization manages its day-to-day expenses. Numerous factors affect operating profit margin. They include the specific mix of payers that the hospital bills—health organizations with a higher percentage of patients insured by Medicare or Medicaid generally have lower operating profit margins than those with a higher percentage of privately insured patients—as well as variations in treatment profitability, costs associated with regulatory compliance, and labor costs. Operating profit margin can indicate areas where cost management or process improvements are needed.
-
Total Profit Margin
Also known as net profit margin, total profit margin is the definitive measure of a company’s profitability, representing the percentage of revenue left after all expenses have been paid. Some of these expenses—such as interest paid on debt—are common to most industries. Others, such as uncompensated care and malpractice insurance, are specific to healthcare. These expenses can vary dramatically from one health organization to another. For example, hospitals that serve low-income communities typically provide more uncompensated care and, therefore, have lower profit margins.
Dashboards are crucial for managing total profit margin. For example, a dashboard that shows consistently high interest payments may prompt a review of the hospital’s debt strategy.
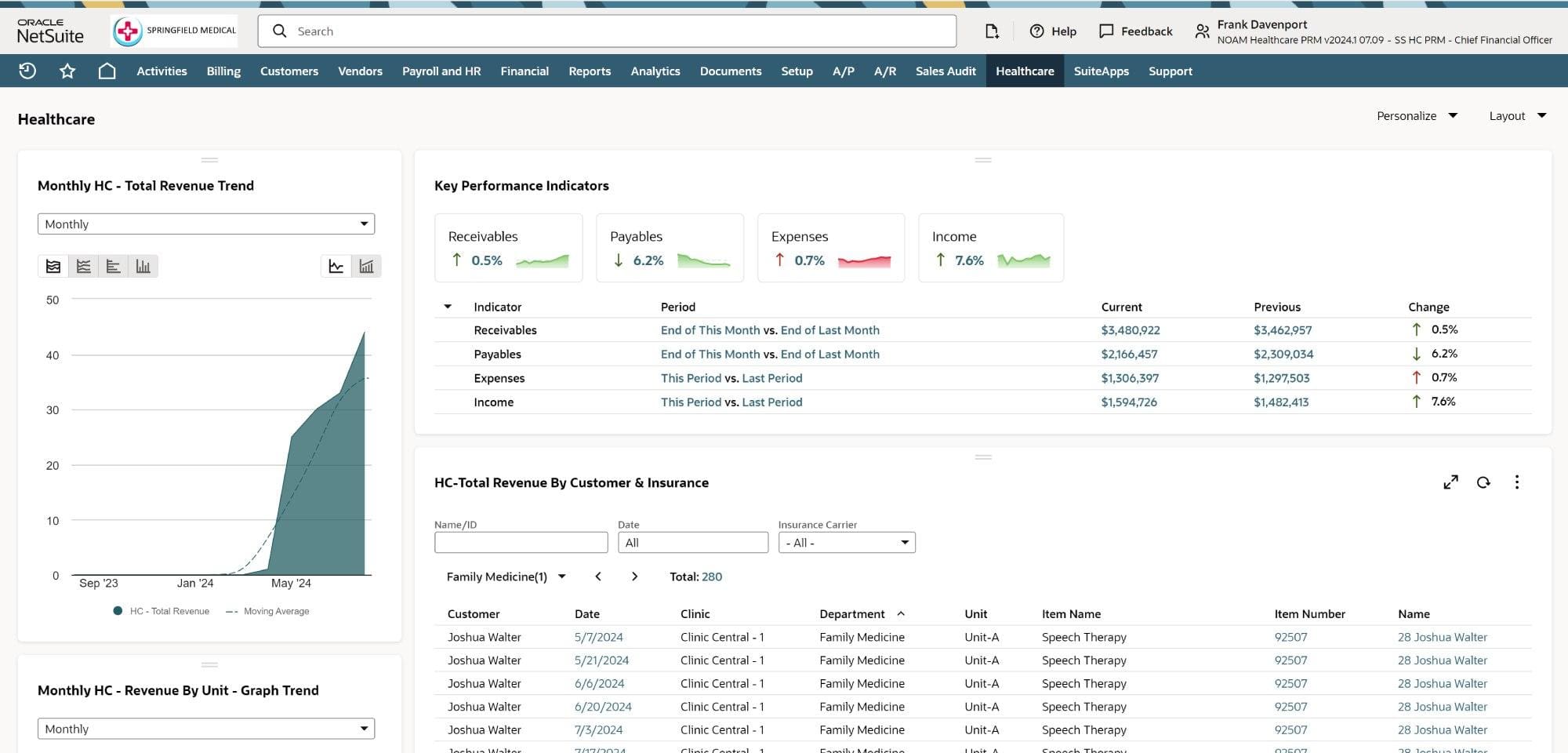
Healthcare Dashboard Example
Healthcare dashboards are designed to give users the data they need to make informed decisions. The following example demonstrate some of the functionality.
Healthcare Success Stories
Healthcare organizations of all stripes share common challenges, such as keeping pace with the volume of constantly changing data across various, and often disconnected, business systems. They must also navigate stringent regulations, protect patient privacy, and maintain the highest standards of patient care. Healthcare dashboards have helped numerous organizations overcome these challenges. Here are three of them.
Crossroads Health
Even within the context of healthcare, the finances for Crossroads Health are complicated. Most of the Ohio-based nonprofit’s $28 million in revenue comes from reimbursements (such as from Medicare) and grants. Not only are grant funds applied to multiple projects, Crossroads also manages labor distributions, splitting individual employee’s time and salary across different grants.
This disbursement introduces its own set of challenges. One is the ability to ensure that every grant dollar is spent, and spent wisely. Another is budgeting, as Crossroads forecasts and tracks allocations within bigger allocations. These challenges were further magnified by its rapid growth: Crossroads doubled in size in just five years.
Reporting these numbers was no easy feat either, until the leadership team began using dashboard data to keep the board informed and also as the basis for proposals to Crossroads’s primary funders. In both cases, dashboard tools kept the data current and easy to interpret.
AyurVAID Hospitals
A lack of centralized data was also a challenge for AyurVAID Hospitals. The organization was caring for 18,000 patients across several facilities in different Indian states. Managing that data manually was labor-intensive and time-consuming, and it was understandably difficult to correlate information from one part of a patient’s life cycle to another.
Thanks to its dashboard, AyurVAID Hospitals is able to follow patients through the entire patient life cycle, from registration and screening to treatment and, ultimately, satisfaction surveys. That data is available in real time to anyone who needs it, at any of the company’s locations. The dashboard benefits reach throughout the operation: The system automates inventory management for more than 750 items; patients can use a self-service portal; and metrics have facilitated continuous improvements in care.
The positive impact on AyurVAID’s bottom line is measurable. After implementing the system, revenue increased 35% in the first two years and another 45% in the third year.
How to Choose the Right Healthcare Dashboard
The “right” healthcare dashboard will meld the organization’s specific goals and the dashboard’s capabilities. The process starts by engaging stakeholders to identify the kinds of dashboards that would help them perform their jobs better. For example, administrators may require an operational dashboard to keep real-time tabs on day-to-day operations, while clinicians on the frontline would need a dashboard that monitors patient vitals, lab results and medication schedules.
Next comes selecting the KPIs that will guide informed decisions across the organization and within individual departments and user groups. This step is followed by locating the necessary data across various business systems and determining its quality and timeliness.
A dashboard can shine a spotlight on the best of all possible data, providing its user interface is easy to use, well organized and visually appealing. Finally, before rolling out the dashboard, have various constituencies make sure it works as intended. Technical glitches should be resolved before full implementation takes place.
Here are a few best practices to keep in mind.
- Make data accuracy and reliability a priority: Ensure that dashboards connect to various data sources, using data cleansing and reformatting capabilities to build on a strong foundation.
- Build strong data security measures: Implement robust security protocols, including user access controls, row-level security and compliance with regulations to protect sensitive information.
- Keep the system flexible—and evaluate it often: Maintain a dashboard system that can scale with organizational growth and adapt to evolving user needs. Conduct periodic needs-and-gaps analyses to maintain effectiveness.
- Ensure that the dashboard integrates seamlessly with existing systems and technologies: Doing so reduces the number of data-entry errors, improves the accuracy and completeness of patient records, and streamlines workflows.
Maximize Profits with NetSuite Healthcare ERP
Healthcare companies gain the greatest value from dashboards that can be adapted to meet changing government regulations, insurance company policies and processes, market conditions, treatment regimens, and other external variables. Other pressures are internal, such as the need to manage growth. Whatever the situation may be, NetSuite’s cloud-based enterprise resource planning (ERP) system for healthcare and life sciences offers the power and flexibility that healthcare companies need.
NetSuite’s ERP provides comprehensive financial management tools that integrate with back-office processes for real-time tracking, reporting, and auditing; integration with customer relationship management applications to capture a complete patient view; and customizable workflows and reporting features. The NetSuite solution also helps ensure data security with strong encryption, robust password policies, multifactor authentication, and access controls.
Navigating the complexities of healthcare data and decision-making is an enduring challenge. A well-designed dashboard simplifies this complexity and helps healthcare professionals at every level make timely, well-informed decisions to help improve the operational “health” of their organizations.
Healthcare Dashboard FAQs
What is the difference between a health dashboard and a personal health dashboard?
In simplest terms, a health dashboard is designed to provide insights across a healthcare population, while a personal health dashboard focuses on managing an individual’s health. Health dashboards are used in a variety of healthcare settings, such as hospitals, nursing homes, large medical practices, and urgent care facilities, as well as by a variety of professionals. In contrast, a personal health dashboard is intended to be used only by individuals to access data about their own health.
What are KPIs in healthcare?
Key performance indicators are specific, measurable metrics used to assess how well an organization is meeting its goals. Healthcare KPIs include patient satisfaction scores, emergency room wait times, claims denial percentage, and cost per treatment.
Why are dashboard metrics important in healthcare?
Streamline and structure data:Dashboard metrics help healthcare organizations track their performance, identify areas for improvement, and make decisions that improve patient care and business operations, all from one centralized location.









