ERP systems are powerful, comprehensive tools often made up of distinct but connected modules for functions such as financial management, human resources (HR), supply chain management (SCM), and customer relationship management (CRM), among other capabilities. There are also industry-specific modules for patient and clinical management that can help healthcare organizations bring order to their operations. Success, however, hinges on selecting ERP modules that will meet each healthcare organization’s unique needs in order to drive essential efficiency and deliver seamless patient care.
What Are ERP Modules?
ERP modules are individual components within a larger ERP system, each designed to manage a specific area of operations, such as finance, HR, or SCM. The power of ERP systems lies in their ability to integrate these modules to create seamless data sharing and limit manual processes. This flexibility of cloud-based systems simplifies IT infrastructure, supports remote work, and ensures that everyone works with up-to-date information.
What Are Healthcare ERP Modules?
Healthcare ERP modules are like the nerve center of a healthcare organization, connected within a larger ERP system to bring together every vital part of operations. These modules include many of the same components of generic ERP systems, such as financial management, HR, CRM, and SCM, but also contain specific capabilities for healthcare organizations, from patient records and medical inventory to billing, staff scheduling, and compliance, keeping the right information flowing to the right people at the right time. Instead of juggling multiple systems, healthcare companies can use these connected modules within a single ERP system to simplify their most complex tasks, such as tracking supplies or processing insurance claims, while automation works quietly in the background to handle the details.
A patient’s medical history stored in one module can instantly inform billing in another, eliminating redundant data entry and cutting down on human error. The result is smoother workflows, more accurate information, and faster decision-making. Cloud-based ERP systems take this one step further: They enable access to critical information from any clinic, hospital, or remote location to provide a more flexible and connected approach to healthcare that not only streamlines operations but also frees staff to focus more on delivering exceptional patient care.
Key Takeaways
- A healthcare ERP module is a specialized software component within an ERP system that manages a specific operational function.
- Healthcare ERP modules improve operational efficiency and data accuracy while simplifying workflows, resulting in smoother operations and higher-quality patient care.
- The top challenges of healthcare ERP modules include high implementation costs, data security concerns, regulatory compliance, workflow disruptions, and integration issues with existing systems.
- Some of the most popular healthcare ERP modules include financial management, patient management, SCM, HR, and clinical management.
- When selecting ERP modules, healthcare companies should assess their specific operational needs, prioritize regulatory compliance, and choose scalable solutions.
Why Are ERP Modules Important in Healthcare?
ERP modules offer healthcare companies a level of efficiency and coordination that older, disconnected software and manual processes simply can’t. Before the advent of ERP systems, healthcare companies were often stuck juggling multiple systems that didn’t speak to each other—one for patient records, another for inventory, and still another for billing, for example. This created information silos, slowed down operations, and increased the chances for error. In healthcare, those errors can come at a high cost, not just financially but with regard to patient care, where even small mistakes can impact lives.
ERP modules eliminate that chaos by integrating everything into a single, streamlined, automated system. With a real-time flow of data, for instance, inventory levels update automatically when supplies are used, so stock can be added to always be available when needed. Billing and insurance claims can be processed minus the headaches of duplicated entries or missed steps. And, thanks to ERP systems, modules for HR processes, such as scheduling, payroll, and compliance, run just as smoothly, so healthcare professionals have more time to devote to patients rather than paperwork.
Advantages of Healthcare ERP Modules Integration
Integrating healthcare ERP modules brings order to disjointed systems and processes, fundamentally improving how healthcare companies operate day to day. Done well, integrated ERP modules don’t just build efficiency; they create a seamless flow of information that allows healthcare professionals to focus on patient care rather than on administrative work. Here are six of the most common benefits of integrated ERP modules in healthcare.
- Improved operational efficiency: In the healthcare industry, where even small delays can have big consequences, healthcare organizations face the constant challenge of managing complex operations without missing a beat. According to a survey by the American Medical Association, 78% of participating physicians said delays in patient authorization sometimes or always led to patients abandoning treatment. By connecting everything from patient records to inventory and billing into one cohesive system, ERP integration eliminates the silos that slow down workflows. For example, an automated inventory system that talks directly to a procurement system can prevent supplies from running out.
- Enhanced data accuracy: Data accuracy can be responsible for the difference between smooth operations and critical errors that impact patient care. When patient records, inventory, and billing data are scattered across multiple systems, mistakes are bound to happen: duplicate entries, missing information, or outdated records slipping through the cracks. With all data residing in one integrated ERP system, however, everything is updated in real time. For example, a patient’s treatment plan is seamlessly linked to billing and insurance information, reducing the chances of errors that lead to claim denials or delays. With integrated ERP modules, healthcare organizations can save time and have confidence in the accuracy of their data, which translates into better decision-making, fewer mistakes, and, ultimately, improved patient outcomes.
- Increased revenue: In healthcare, increasing revenue is about cutting costs and improving efficiency so more resources can go where they’re needed most: patient care. ERP modules help drive revenue growth by optimizing every part of the operation, from billing and claims processing to inventory management. When financial processes are automated and streamlined, claims are submitted faster and reimbursements happen on time. For example, a hospital using an integrated ERP system can track patient treatments in real time, automatically generating accurate billing codes and invoices. The results are fewer billing errors, faster payments, and more revenue flowing back into the organization—all while maintaining a high standard of care.
- Stronger compliance and security: Compliance and security are nonnegotiable in healthcare, where patient privacy and regulatory requirements are tightly intertwined. Keeping up with constantly evolving regulations, such as the Healthcare Insurance Portability and Accountability Act (HIPAA), can feel like an uphill battle, especially when using disjointed systems. Healthcare ERP modules create a unified platform that automates compliance checks and enforces security protocols across the entire operation. Instead of relying on manual processes to track regulatory changes, an integrated ERP system can automatically update and apply the latest rules, reducing the risk of costly violations. For example, patient data can be securely stored and accessed in a way that meets all privacy standards, with real-time monitoring and audit trails ensuring that compliance is built into everyday operations.
- Data-driven decision-making: In healthcare, decisions need to be quick, informed, and backed by solid data. But when information is scattered across different systems, it’s hard to get a full picture in real time. ERP modules aggregate critical data from patient records, financials, and inventory into a single platform for a clear, up-to-the-minute view of operations. As a result, healthcare companies can make smarter, faster decisions. For example, with real-time insights on patient volumes and staffing needs, a hospital can quickly reallocate resources to meet demand and sidestep bottlenecks, leading to better patient care. The result is a shift from reactive to proactive operations, using data to make decisions that not only solve immediate problems but also anticipate future needs.
- Better patient care: Better patient care is the ultimate goal of every healthcare organization, and ERP modules play a key role in making that a reality. When systems are fragmented, critical information can get lost in the shuffle, delaying treatments or causing errors that impact patient outcomes. By integrating everything from patient records to scheduling and billing, ERP modules optimize the flow of information across departments so that healthcare providers always have access to accurate, up-to-date data. If a doctor needs immediate access to a patient’s medical history during an emergency, an ERP system makes that possible in seconds, facilitating faster, well-informed treatment decisions.
Challenges of Healthcare ERP Module Integration
Integrating healthcare ERP modules promises smoother operations, but if not executed well, the road to getting there can be full of obstacles, including costly implementations and workflow disruptions. Understanding the following potential challenges is the first step to overcoming them and unlocking the full potential of an integrated ERP system.
- Implementation costs: Implementing ERP modules in healthcare is no small feat. It can come with a steep price tag and unique challenges, particularly with on-premises systems that require large up-front investment in hardware, software, and IT resources. Healthcare organizations, already juggling tight budgets and complex operations, can find the transition costly. A report from Definitive Healthcare notes that average hospital operating profit margins in 2022 were actually a loss of 3.8%. Unexpected ERP implementation costs can include migrating patient records, integrating with existing technologies, building customizations, and keeping staff fully trained. Though the long-term payoff is clear, the up-front investment can be a difficult hurdle to overcome. Cloud-based ERP systems can significantly reduce these up-front costs, because healthcare companies don’t need to purchase hardware and software, which are handled by a cloud provider.
- Data security concerns: As discussed earlier, data security is a top priority for healthcare organizations, and although ERP systems can improve overall data security, success relies on strong integrations. Any misstep could expose critical data to risks, like breaches or unauthorized access, especially for companies moving from older, legacy systems to a modern ERP platform. According to the HIPAA Journal, 2023 was a record-setting year for healthcare data breaches. Not only did the industry record its highest number of data breaches, but it also set a record for most records exposed. Older systems may not have the same security standards, which could render the data transfer process vulnerable. Hospitals upgrading to integrated ERP systems might need to invest in robust encryption and security protocols to protect patient records during migration.
- Regulatory compliance: Navigating regulatory compliance during ERP implementation in healthcare is like walking a tightrope. Organizations have to make sure that patient data flows through their systems in ways that meet strict regulatory requirements, like those mandated by HIPAA and the Trusted Exchange Framework and Common Agreement (TEFCA). Any misalignment can result in costly fines—or worse yet, compromised patient care. For example, ensuring that only authorized personnel can access sensitive medical records and tracking every interaction for audits can add layers of complexity. The more this can be automated within an ERP system, such as by automatically applying the latest compliance rules across all data touchpoints, the smoother and safer data management becomes. This is another benefit of cloud-based systems, which are updated automatically by the ERP provider to maintain compliance with the latest rules.
- Integration issues: Integration issues are a common challenge when implementing ERP systems in healthcare, especially when trying to connect the new solution with legacy systems. Older systems might not be designed to sync seamlessly with modern ERP systems, leading to data inconsistencies or gaps in functionality. For example, a hospital might struggle to integrate its existing patient management system with a new ERP system, causing delays in accessing critical data. Without careful planning and testing, this can slow down operations and create more headaches than the ERP system was meant to solve.
- Workflow changes: Implementing an ERP system often brings significant changes to workflows, especially in a clinical setting. For example, staff who are used to accessing information through separate, department-specific systems may suddenly need to navigate a unified ERP solution, which changes how they search for, input, and manage data. While these changes are designed to improve efficiency and data accessibility in the long run, the adjustment period can create bottlenecks while employees learn the new system. It’s a temporary hurdle but one that can cause disruptions if not carefully managed during implementation.
- Allure of customization: Software customization can be a temptation to healthcare organizations, because each department in the company often has its own unique needs. The desire to tailor ERP modules for every specific use case, however, can quickly spiral into complex, costly adjustments that delay implementation and complicate future updates. Though customization offers a tailored fit, it’s important to strike a balance with regard to the benefits of standardization, which allow for smoother integration and easier maintenance down the line. For example, a standardized approach grants quicker upgrades and presents fewer compatibility issues, so the organization remains agile as technology evolves.
- Potential operational disruptions: Implementing an ERP system can lead to temporary operational disruptions, especially during the transition phase. As old systems are phased out and new workflows are introduced, short-term delays in accessing critical information or completing tasks may occur. For instance, as a hospital upgrades its ERP system, staff might face downtime or slower response times that can affect scheduling, billing, and patient care. Though these disruptions are usually temporary, careful planning and continued communication are needed to minimize their impact on day-to-day operations.
Top 10 Healthcare ERP Modules and Features
Understanding the most common healthcare ERP modules and their features is essential for building a system that not only supports daily operations but also improves patient care and overall efficiency. Each of the following modules plays a potentially critical role in keeping everything running smoothly.
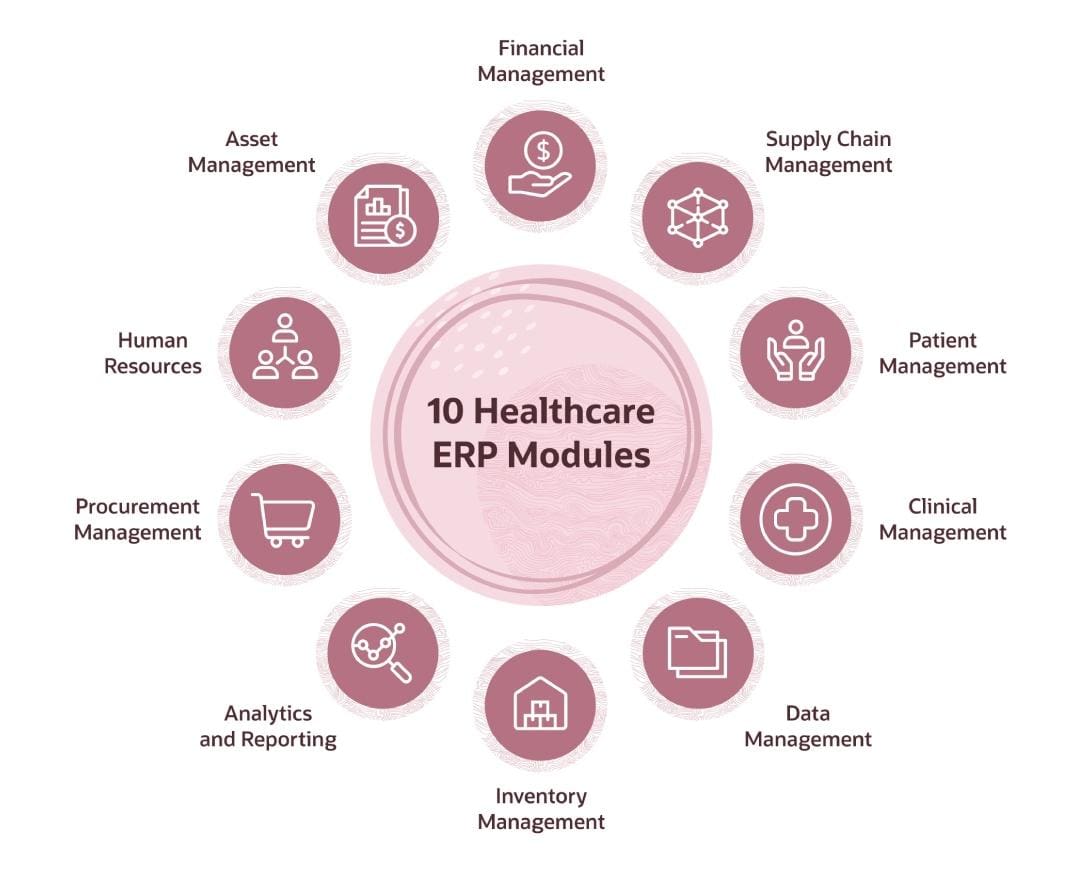
1. Financial Management
Managing finances in healthcare can be a complex balancing act, with hospitals and clinics needing to simultaneously track revenue, expenses, insurance claims, and regulatory compliance. A financial management module helps healthcare organizations keep these moving parts in sync by offering real-time insights into cash flow, budgeting, and financial performance. Key features to look for in a financial management module include automated billing, accounts payable/receivable, and integration with insurance claims systems to reduce errors and speed up payment processing. Also look for financial reporting and regulatory compliance tools to keep up with industry standards, such as HIPAA.
2. Supply Chain Management
An SCM module helps healthcare companies stay on top of the complex process of managing the flow of medical supplies, equipment, and pharmaceuticals. It tracks everything from procurement purchases to inventory levels, so essential items are always available when needed without overstocking, which ties up money that could be used more effectively elsewhere. An SCM module should include automated inventory tracking, vendor management, and real-time supply monitoring, all features that help healthcare providers avoid shortages, reduce waste, and optimize ordering processes.
3. Patient Management
A comprehensive patient management module streamlines workflows, giving healthcare professionals more time to focus on delivering high-quality care. It centralizes patient records, appointments, treatment histories, and discharge summaries, making it easier for staff to access up-to-date information as needed. The patient management module should offer scheduling, real-time patient tracking, and seamless integration with electronic health records (EHR) systems. This Integration reduces the likelihood of errors, improves care coordination, and helps providers offer a smoother patient experience.
4. Clinical Management
A clinical management module is at the heart of healthcare operations, managing and coordinating all aspects of patient care, including treatment plans, lab results, medication management, and clinical workflows. Most important, this module gives medical staff immediate access to vital patient information. Most clinical management modules include tools for documenting care, tracking patient progress, and managing clinical resources in real time. As a result, clinicians can make faster, smarter decisions that reduce the risk of errors in treatment.
5. Data Management
Managing vast amounts of healthcare data—think patient records and operational metrics—can seem overwhelming without the right tools. A data management module helps healthcare organizations organize, store, and access critical data efficiently, which is crucial for improving operational performance and patient care quality. Whether tracking patient outcomes or analyzing trends in care delivery, the data management module provides a single source of truth for all data-related needs and fuels seamless data integration across departments, so teams have the insights they need to make evidence-based decisions.
6. Inventory Management
Keeping track of medical supplies and equipment is no small task. Healthcare organizations handle a staggering array of items with varying shelf lives and usage rates, not to mention their level of critical importance to patient care. An inventory management module helps monitor stock levels, manage orders, and track the usage of key supplies so items are always available without creating waste. Though its focus is on internal stock control, this module works in tandem with the broader SCM module, which oversees procurement and vendor relationships. Instead of relying on manual tracking or disconnected systems, an inventory management module provides real-time updates on what’s in stock, what’s been used, and what needs replenishing. The result is fewer shortages and less over-ordering.
7. Analytics and Reporting
Analytics and reporting modules are essential for turning raw healthcare data into actionable insights. In an environment where every decision can affect patient care and operational efficiency, the ability to quickly analyze and report on data is of prime importance. This module helps healthcare organizations track performance metrics, identify trends, and make evidence-based decisions that improve clinical and administrative processes. Unlike manual reporting, which can be time-consuming and prone to errors, an analytics and reporting module automates the collection and analysis of data to deliver real-time insights that allow healthcare organizations to make informed decisions that drive better outcomes.
8. Procurement
A procurement module plays an important role in managing the way healthcare organizations purchase the supplies, equipment, and services they need to operate smoothly. It centralizes and streamlines the entire purchasing process—from sourcing medical equipment to negotiating vendor contracts—and automates tasks, such as purchase-order approvals and vendor management, to make ordering supplies more efficient and cost-effective. Unlike spreadsheet-driven procurement processes that can lead to delays or overspending, a procurement module provides real-time visibility into spending, vendor performance, and order status, which controls costs, avoids supply disruptions, and keeps the focus on delivery of high-quality care.
9. Human Resources
Healthcare organizations face unique resource challenges, such as juggling complex staff schedules, maintaining up-to-date certifications, and monitoring compliance with regulations. Managing a diverse workforce comprising doctors, nurses, administrative staff, and specialists requires precision—even small mistakes can lead to gaps in care or costly compliance failures. An HR module streamlines employee-records management, automates payroll, and tracks certifications, which means qualified staff are always in place.
10. Asset Management
Healthcare companies deal with a wide range of assets, including expensive medical equipment like magnetic resonance imaging machines and everyday tools like wheelchairs and infusion pumps—all of which need to be properly maintained and available at a moment’s notice. The challenge isn’t just keeping track of these assets but also making sure they’re regularly serviced, fully operational, and compliant with regulatory standards. An asset management module monitors the life cycle of equipment, schedules maintenance, and tracks the location and status of assets in real time. The result is less equipment downtime, longer equipment lifespans, and tools that are always ready when patients need them.
How to Select Healthcare ERP Modules
Each healthcare organization will have its own unique needs when it comes to ERP modules. The following eight steps can help identify those needs and focus the evaluation process on solutions that address them.
- Assess organizational needs: The evaluation process starts by pinpointing unique needs. Identify gaps in current systems and processes and prioritize areas where ERP modules can provide the most value.
- Involve key stakeholders: Bring together department heads, clinical staff, and IT professionals to gather a wide range of perspectives. Their input will help identify modules that align with both operational and clinical workflows.
- Evaluate scalability: ERP modules must evolve as organizations grow. Whether the target is new services or fresh locations, modules should be flexible enough to scale as needs change.
- Check for integration capabilities: Look for ERP modules that integrate smoothly with existing systems, such as EHR or financial platforms. Seamless integration minimizes disruptions and keeps data flowing easily among platforms.
- Prioritize compliance features: It’s important for ERP modules to meet regulatory requirements, such as those from HIPAA and TEFCA. Automated compliance features save time and diminish the risk of errors in patient data management.
- Consider user experience: Choose modules that are intuitive and easy for staff to use. The faster teams adapt to the new system, the sooner efficiency and care will improve.
- Focus on data security: Select a system with robust security features to protect sensitive patient information. Encryption, access controls, and audit trails should be standard to safeguard data.
- Look at vendor support: A reliable vendor offers more than just software; it provides ongoing support and training, as well. Look for vendors with a strong track record for helping healthcare organizations through implementation and beyond.
Optimize Healthcare ERP Operations With NetSuite
NetSuite’s ERP solutions offer healthcare companies a flexible, cloud-based platform designed to simplify operations and improve financial visibility. With features such as real-time data access, automated billing, and seamless integration with existing systems, NetSuite helps healthcare organizations reduce inefficiencies and improve decision-making. Its unified solution simplifies everything from financial management to supply chain and procurement, all while guaranteeing regulatory compliance.
Because it’s cloud-based, NetSuite ERP allows healthcare providers to access critical information from anywhere, facilitating remote work and more responsive care. NetSuite also offers scalability, making it ideal for healthcare companies looking to grow or expand their services without having to overhaul their systems in the process. By centralizing data and automating processes, NetSuite helps healthcare organizations operate more efficiently to focus on delivering high-quality care.
Choosing the right ERP modules for a healthcare organization isn’t just about improving efficiency; it’s a critical component of successful care delivery. When the right systems are in place, doctors, nurses, and administrators can focus less on paperwork and more on patients—an absolute necessity in a field where time and accuracy can mean the difference between life and death.
Healthcare ERP Modules FAQs
What is the difference between ERP and EHR?
Enterprise resource planning (ERP) systems are designed to manage the business operations of an organization, including finance, procurement, supply chain, and human resources. Electronic health records (EHR) systems focus specifically on managing patient-related information, such as medical histories, treatments, and care plans. While ERP solutions simplify operational and administrative processes, EHR systems are essential for improving clinical workflows and patient care. Both can work together in healthcare settings, but they serve distinct functions.
What is the most common ERP module in healthcare?
The most common enterprise resource planning (ERP) module in healthcare is the financial management module. Healthcare organizations rely heavily on this module to handle billing, budgeting, and accounts payable/receivable. Given the complexity of healthcare billing and insurance claims, financial management is essential to keep cash flow steady and alleviate administrative burdens.
What is the best ERP for healthcare?
The best enterprise resource planning (ERP) system for a healthcare company depends on their specific needs, encompassing factors like company size, complexity, and long-term goals. An ideal ERP system should offer comprehensive features, such as financial management, supply chain integration, and strong regulatory compliance tools. Cloud-based options provide flexibility, and customizable solutions can adapt to the unique workflows of different healthcare providers. Ultimately, the best ERP system is one that aligns with an organization’s operational needs and helps improve efficiency and patient care.









